The Morning After Pill
Contraceptive controversies abound in the discussion over whether or not to offer emergency contraceptive pills to students.
Pittsburg State University, 45 minutes from Missouri Southern’s campus, has been offering students the morning-after pill for years. Prescriptions are available through the health center for $30 after a pregnancy test is confirmed negative. The student must return for an appointment one week after her period was to begin and undergo an additional pregnancy test.
Jan Dipley, Southern’s health services director, thinks Southern should offer the pill, but the decision is not up to her. In Missouri, nurse practitioners must practice under the supervision of a physician in that specialty. The doctor supervising Southern’s health center made the decision that Dipley and the rest of the health center staff are not allowed to prescribe the morning-after pill because it would increase Southern’s liability.
Dipley doesn’t think that makes sense because the majority of students are over 18 years old. Instead, when students come to the health center requesting ECPs, the staff refers them to Joplin’s Family Planning Clinic.
“I fully believe that it’s a woman’s right and her choice to be protected if she chooses to not abstain,” Dipley said. “But we decided it was just as easy to send them [students] to Family Planning.”
Dipley said some students from overseas were surprised the United States does not sell ECPs over the counter like their home countries. The Food and Drug Administration decided earlier this year to deny a laboratory’s application to sell ECPs over the counter in an apparent contradiction to the recommendations of two FDA advisory panels that voted 23-4 in December 2003 to sell Plan B, a progestin only ECP, without a prescription.
Dipley believes ECPs should be sold without a prescription and one reason it is not being offered to Southern’s students is the conservative nature of the region.
“This is the Bible Belt, but sex should be more out in the open,” she said. “It should be a personal choice. How can they [students] make an informed choice if they aren’t aware of what’s going on?”
Many people are in opposition to ECPs after confusing them with other controversial birth control methods, like RU-486 – the abortion pill.
Sally Pace, clinic manager of women’s health and family planning emphasizes the differences between the two pills.
“When it first came out, everyone said it was an abortion pill, but there’s a big difference,” Pace said.
RU-486, mifepristone, also referred to as the abortion pill or chemical abortion is not the morning after pill. Mifepristone is approved for early abortions in the United States and several large European countries. It is only available as an emergency contraceptive in China. RU-486 can only be taken four to seven weeks after a woman’s last missed period.
The process involves a series of pills. The first, Mifepristone, depletes the lining of the uterus preventing the pregnancy hormone progesterone from working and causes the blood supply to the embryo to shut off and the fetus to die. Two days later, a second pill, prostaglandin, is taken to induce labor and expel the fetus. Side effects of RU-486 include nausea, cramps and bleeding.
On the other hand, there are two forms of ECPs. One uses hormones similar to ordinary birth control pills, estrogen and progestin, but in higher doses. The Emergency Contraception Website, operated by the Office of Population Research at Princeton University and the Association of Reproductive Health Professionals, said these types of pills cause nausea in 50 percent of women and vomiting in 20 percent. The other type of ECP, contains only progestin and is more effective and less likely to cause nausea or vomiting. The pills must be started within the first 120 hours after unprotected sex.
ECPs work in three different ways. They inhibit or delay ovulation in 75 percent of the women who take them. The pills also form a thick mucus blockade around the cervix, preventing the sperm from fertilizing the egg, and alter the lining of the uterus to make it harder for the egg to implant. Most people have a problem with the third method of preventing pregnancy.
The debate reaches full force when physicians and care-givers attempt to define the beginning of life. Sharon Keogh, nurse practitioner of women’s health and family planning, said ECPs are for use “before pregnancy is determined” and ordinary birth control pills are “to prevent pregnancy to begin with.”
The question becomes whether ECPs prevent conception or implantation. Does the morning-after pill impede sperm from reaching the egg or instead prevent a fertilized egg from implanting and growing into a baby?
Debra Miller, Lifechoices clinic nurse manager, said physicians can legally say ECPs prevent pregnancy and do not abort a fetus because the medical definition is implantation and not conception even though at fertilization the baby’s features, including sex, hair and eye color, have already been determined.
“Things can either be alive or not,” said Miller.
“I have no doubt that life begins at conception and not at implantation,” said Rita Lawson, Lifechoices client services director.
The possibility of an “unfriendly uterus” preventing pregnancy has been suggested by the FDA since the beginning, but is considered unlikely by researchers and the idea of unintentional abortions appears to be extremely remote.
Pace said the clinic offers the pill to anyone who needs it and said despite the hype, ECPs are not that prevalent in the area.
“They made such a big deal about it and its not,” Pace said. “Contraception is so available now that it’s not a big deal.”
Regardless of the moral issues raised by the controversy, all parties involved can agree on one thing. ECPs are for emergencies and not meant as a way of life.
“We’re not looking at this as a form of birth control, it’s literally an emergency contraceptive for rare occasions when the condom breaks or they forget to take their pills,” Keogh said.
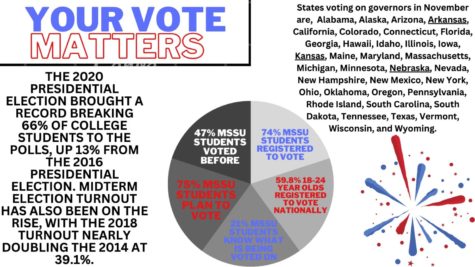
Your donation will support the student journalists of Missouri Southern State University. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.